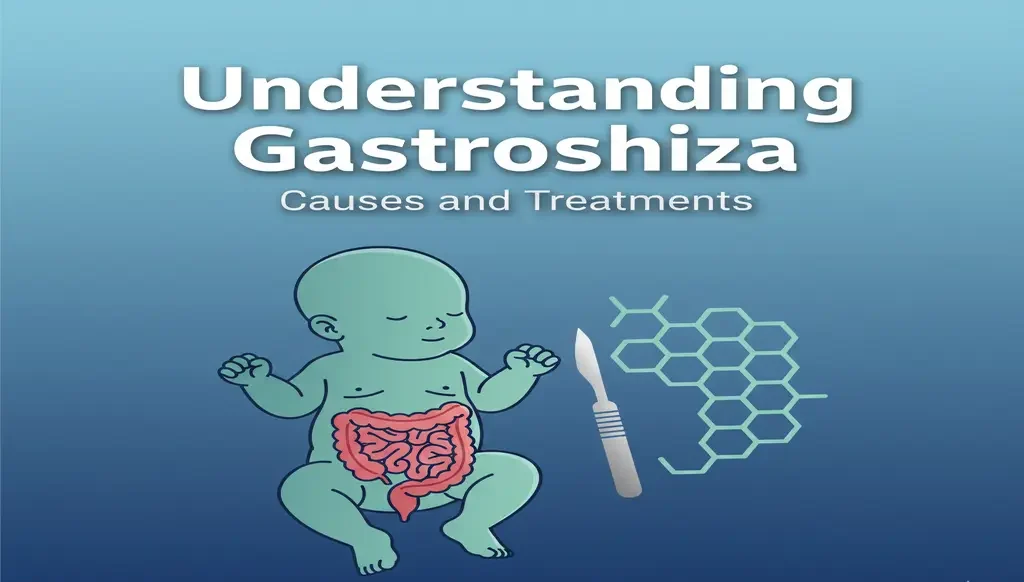
Gastroshiza is a critical ailment that is present in infants. The condition is characterized by an abdominal wall defect. Thus, the intestines can come out of the body through the opening.
To be able to cope with gastroshiza, the parents and caregivers need to have a good understanding of the problem. If the diagnosis and treatment are done early enough, the outcomes will be positively affected significantly.
Surgery for gastrochisis is the main treatment option. It includes the procedure of placing the intestines back inside the abdomen. The child’s condition will determine the timing and the method.
Parents usually go through a hard time both emotionally and practically. Support and resources are essential for helping them through this journey.
This piece of writing looks into the reasons behind gastroshiza, its detection, and treatment. It is meant to be a comprehensive source of information for the affected.
What is gastroshiza?
Gastroshiza is a congenital defect that is noticeable at birth. It happens when a hole around the umbilicus results in the intestines being outside the body and exposed. This condition is an abdominal wall defect.
In most cases, the diagnosis is a shock to the parents. On the contrary, being aware of the truth is giving power. With gastroshiza, the abdominal wall is incompletely formed during the growth of the fetus.
In a good number of cases, gastroshiza is able to be diagnosed even before the baby is born. The problem is usually revealed by a prenatal ultrasound. This early detection gives the medical teams time to arrange for instant care right after the baby is delivered.
Here are key features of gastroshiza:
- Intestines protrude outside the body
- Lack of protective sac covering organs
- Can involve other organs like the stomach or liver
While the exact cause remains unclear, genetic and environmental factors may play a role. Thankfully, advanced medical techniques offer effective treatment options. A collaborative approach ensures comprehensive care for the newborn and peace of mind for parents.

Causes and Risk Factors of gastroshiza
The exact origins of gastroshiza are still pretty much a mystery. Nevertheless, it seems to be the result of a complicated interaction between genetic and environmental factors. Even though no one gene has been indicated, family background may be a factor to increase the likelihood.
Some risk factors have been pointed out that might raise the chances of a child with gastroshiza being born. One of the most critical risk factors is the young age of the mother. It is more common in mothers under the age of 20.
Another factor of lower socioeconomic status is associated with higher incidence rates. The relationship implies that differences in lifestyle or prenatal care might affect the results.
Pregnancy-related behaviors might also be factors. The maternity-related factors such as smoking and using drugs are being looked at for their possible negative effects. Plus, the question of insufficient prenatal nutrition is also being raised.
Factors associated with gastroshiza include:
- Young maternal age
- Lower socioeconomic status
- Possible family history
- Lifestyle choices such as smoking
Ongoing research is crucial to unraveling the exact causes of gastroshiza. As we improve our understanding, this knowledge could lead to better preventive measures.

How is gastroshiza Diagnosed?
Gastroshiza is generally diagnosed after pregnancy, via standard prenatal ultrasound scans. The case is very obvious because the intestines are positioned exterior to the baby abdomen. The defect’s major characteristic gives the medical staff a chance to identify it with high accuracy.
The early diagnosis is of great importance for quality baby care planning. It allows the doctors to create a management and treatment plan that fits the situation best before the baby is born. Such planning is a must for delivering quick and efficient intervention when the baby is born.
An ultrasound scan can show numerous signs that gastroshiza may be present. Typically, these signs are substantiated through additional imaging or testing if necessary. A thorough assessment also helps to exclude other diseases or complications.
Common diagnostic steps include:
- Routine prenatal ultrasound
- Detailed fetal imaging
- Follow-up ultrasounds
After birth, a physical examination confirms the diagnosis. This final step is necessary to assess the severity and plan the immediate next steps.
Symptoms and Immediate Concerns After Birth
The protrusion of the intestines through the abdominal wall is the most evident symptom of gastroshiza at birth. It is a condition characterized by the lack of a protective covering over the exposed organs, thus making them at risk.
The immediate concerns involve the chance of infection and the risk of damage to the intestines that are out. Medical attention must be sought urgently in order to avoid complications. Meticulous management is important to keep the organs sterile and hydrated.
The healthcare providers’ first priority is to stabilize the baby. They are going to work fast to start the protective measures and to make a plan for the corrective surgery. These first actions are very important not only for the baby’s health in the short term but also for his recovery in the long run.
Key concerns after birth:
- Infection prevention
- Protecting exposed intestines
- Immediate preparation for surgery
The baby is usually transferred to a neonatal intensive care unit (NICU) for specialized care. Continuous monitoring and support help manage the condition effectively in the critical early days.
Treatment Options: Focus on gastrochisis surgery
Gastrochisis surgery is the main treatment for newborns with gastroshiza. The main aim of the operation is to put the intestines that were exposed back into the abdominal cavity in a safe manner.
The surgery will be done depending on the situation of the newborn baby. The surgeons have to be fast but at the same time very careful. If the situation is very urgent, the surgery is done immediately to ensure the baby’s health is safe.
There are generally two surgical methods: primary closure and staged surgery. In primary closure, the intestines are returned, and the defect in the abdominal wall is closed in one operation.
In a case where the defect is too large for starting closure right away, the silo technique might be used. A mesh silo is gradually pushing the organs back into the abdomen over a period of several days.
Common surgical approaches include:
- Primary Closure: One-step surgery
- Staged Repair: Gradual reduction using a silo
- Mesh Silo: Used for large defects
The child is under meticulous scrutiny in the NICU after surgery. The medical teams concentrate on the proper working of the intestines. This attentive treatment contributes to the healing process of the infant.
Gastrochisis operation’s success is greatly attributed to the abilities and the teamwork of the various specialists involved. Obstetricians, surgeons, and NICU personnel work hand in hand. The totality of their expertise gives the baby a greater chance of having a good health outcome.
by National Cancer Institute (https://unsplash.com/@nci)
Post-Surgical Care and Recovery for the Child
After the gastrochesis operation, the little one’s healing process takes place in the neonatal intensive care unit (NICU). Specialized care is given to monitor their condition and deal with any problems that may arise.
One of the most important things in post-operative care is feeding and nutrition. At first, the baby might need to be fed only through IV fluids to get the necessary nutrients while his or her intestines are getting better.
Gradually, breastfeeding or formula feeding can be started as the baby’s digestive system starts to operate normally again. The switch from IV feeding to oral feeding has to be done with great caution.
Important considerations in post-surgical care include:
- Nutritional Support: Starting with IV fluids
- Infection Monitoring: Preventing potential infections
- Pain Management: Ensuring the child’s comfort
Pain management is also a key focus during the recovery period. Medical staff use appropriate interventions to keep the child comfortable and reduce pain levels.
Parents are encouraged to stay involved in their child’s care. The healthcare team will guide them in understanding their child’s needs and recognizing signs of potential issues.

Long-Term Outlook and Potential Complications
In general, the long-range outlook for kids who have surgery for gastrochisis is positive. The majority of kids grow up normally and have good health. But they may still have some problems during their development.
It should be noted by the parents that digestion problems might be one of the issues faced by some of the kids. In this case, feeding, nutrient absorption, or bowel function might be problematic. It is through regular healthcare provider appointments that one can see the best way to deal with these problems.
Potential complications to be mindful of include:
- Digestive challenges
- Growth delays
- Recurrent infections
Even though these issues might occur, they are usually able to be reduced a lot with proper care and medical help at the right time. Early intervention and constant medical assistance are vital for the child to get the best development and health possible. Parents have to keep in touch with the medical professionals to properly deal with any new problems that might come up.
Support for Families and Resources
For families, the emotional burden of gastroshiza can be extremely difficult to handle. Offering guidance, and comfort networks are indispensable. Emotional and practical help should be the main focus of families when it comes to resources.
Gastroshiza has become an issue for many organizations providing support to families. The support groups help parents get in touch with other people who know exactly what they are going through. This type of interaction not only gives emotional support but also offers the sharing of tips and tricks for condition management.
Resources for families include:
- Counseling services
- Support groups
- Educational materials
Families’ burdens can be lightened if they make good use of the resources that are at their disposal. Parents who are provided with enough information and support can be in a position to take the best decisions regarding their child’s treatment. The children and their families alike can also experience an increase in their overall well-being if they interact with these resources.
Frequently Asked Questions about gastroshiza
Gastroshiza often raises many questions for parents and caregivers. It’s essential to have clear, concise answers to help navigate this journey.
Some common questions include:
- What causes gastroshiza?
- Can gastroshiza be prevented?
- What are the immediate steps after diagnosis?
- Will gastroshiza affect my child’s future development?
- How successful is gastrochisis surgery?
Knowing the answers to these questions helps families feel informed and prepared. Having reliable information at hand can alleviate concerns and help in making sound decisions about care and treatment.
Conclusion
Gastroshiza is a difficult condition, however, if it is diagnosed and treated early it gives a good prognosis. It is very important to know the causes, symptoms, and treatments for proper management.
Parents should always ask for help and keep themselves updated to make sure their child gets the best possible treatment. Progress in medical science has been a significant factor in the improvement of life quality for the little ones with gastroshiza. When there is a collaboration and immediate intervention, it is often the case that the affected kids live a healthy and happy life.