Your four-year-old breathes through her mouth constantly. She snores louder than your partner. She’s had three ear infections in six months. The pediatrician mentions “adenoidid” or “enlarged adenoids” and suddenly you’re Googling at midnight, trying to understand what’s happening in your child’s throat.
Adenoidid implies the issue connected with the adenoids—the tiny tissue pads located behind the nose, which, when swollen or infected, can pose serious health risks. Getting to know when these tissues should be treated, the types of treatments available, and what signs indicate critical problems, makes dealing with adenoid issues much easier.
Let me simplify the whole thing for parents and adults facing adenoid issues and present it to them without the medical jargon that makes most health articles unreadable.
What Adenoidid Actually Means
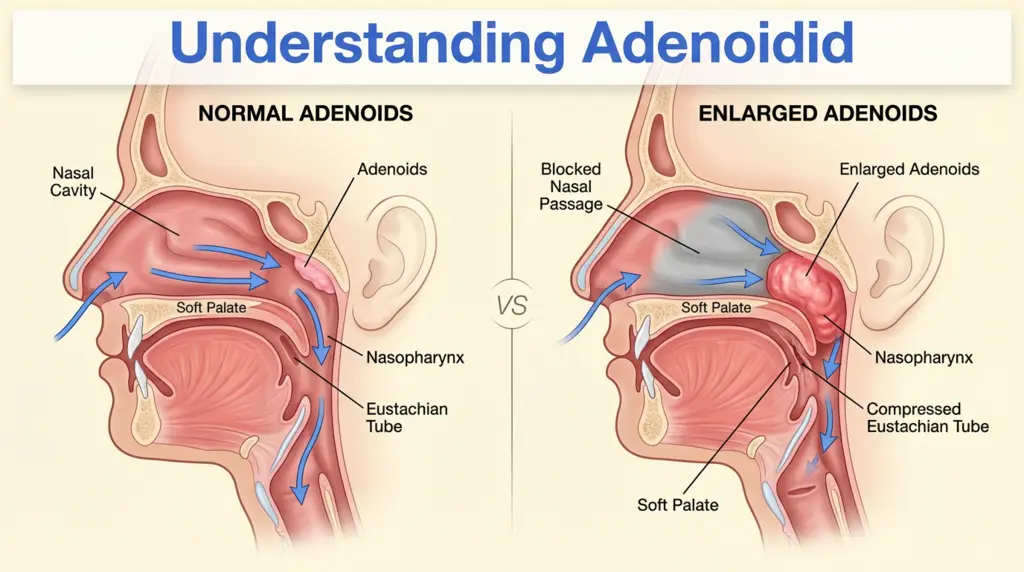
The term “adenoidid” typically refers to adenoid-related problems, particularly adenoid enlargement (adenoid hypertrophy) or inflammation (adenoiditis). These are tissues that sit behind your nasal cavity, above the roof of your mouth, where your nose connects to your throat.
Think of adenoids as immune system guards posted at a strategic entrance. They trap bacteria, viruses, and other pathogens trying to sneak into your body through your nose. When they’re working properly, you never notice them. When they’re not—either because they’ve become enlarged, chronically infected, or just bigger than your anatomy can handle—they create problems ranging from annoying to serious.
Why children are affected more than adults: Adenoids are largest between ages 3 and 7, then gradually shrink throughout childhood. By adulthood, most people have very small adenoids or none at all. That’s why this is primarily a pediatric concern, though adults with persistent adenoid tissue can absolutely experience similar issues.
The confusion around “adenoidid” likely stems from medical terminology. Doctors use specific terms like adenoiditis (infected adenoids), adenoid hypertrophy (enlarged adenoids), and adenoidectomy (surgical removal), which all sound similar but mean slightly different things.
How to Actually Recognize Adenoid Problems
Forget the medical textbook descriptions. Here’s how adenoid issues show up in real life.
Breathing becomes work instead of automatic. Healthy children breathe effortlessly through their noses without thinking about it. When adenoids enlarge enough to block nasal passages, kids adapt by breathing through their mouths—constantly. You’ll notice their lips stay parted even when relaxed, and they might seem like they can never quite catch their breath.
Sleep turns chaotic. Enlarged adenoids don’t just cause occasional snoring. They create loud, persistent snoring every night, sometimes accompanied by brief pauses in breathing (sleep apnea episodes). Kids wake up frequently, though they might not remember it. Morning exhaustion becomes normal despite seemingly “sleeping” 10-12 hours.
Ear infections become a pattern. One or two ear infections per year are common in young children. Five or six infections in a year signals a different problem. Adenoids sit near the Eustachian tubes connecting your middle ear to your throat. When swollen, they block proper drainage, creating perfect conditions for bacterial growth and repeated infections.
Speech sounds different. Chronic nasal blockage changes how children (and adults) sound. Words come out with a “talking through your nose” quality that persists even when they don’t have a cold. Consonants like “m” and “n” sound particularly affected.
The face adapts—and not in good ways. This sounds dramatic but it’s real: chronic mouth breathing during developmental years can actually change facial structure. Dentists call it “adenoid facies”—a characteristic look including elongated face shape, high arched palate, and dental crowding. This happens because constant mouth breathing affects how facial bones grow during childhood.
When Adenoidid Becomes a Medical Concern
Not every child with large adenoids needs treatment. Some kids have naturally larger adenoids that cause zero problems. Others have “normal-sized” adenoids that still block their specific anatomy enough to create issues.
Doctors consider treatment when adenoid problems cause functional impairment—meaning they’re actively interfering with health, development, or quality of life.
Sleep-disordered breathing tops the concern list. If your child stops breathing repeatedly during sleep (observable pauses of 10+ seconds), snores so loudly neighbors can hear, or seems exhausted despite adequate sleep time, that’s not something to “wait and see” about. Sleep apnea in children affects growth, learning, behavior, and cardiovascular health.
Chronic ear infections with hearing impact matter more than occasional ones. Fluid sitting in the middle ear for months prevents the eardrum from vibrating properly, which directly affects hearing. Young children learning language need clear hearing. Persistent fluid buildup from blocked Eustachian tubes (thanks to swollen adenoids) creates a medical indication for intervention.
Growth and development delays raise red flags. Kids who can’t breathe well can’t eat well. Kids who don’t sleep well don’t grow normally. If a child falls off their growth curve or shows developmental delays potentially linked to sleep issues, adenoids become a higher priority concern.
Quality of life counts too. Sometimes the issue isn’t life-threatening but significantly affects daily functioning. A child who can’t participate in sports because they can’t breathe through their nose, or who’s socially isolated because peers tease their snoring at sleepovers, or who’s constantly exhausted and irritable—these quality of life factors legitimately influence treatment decisions.
Conservative Treatment Options That Actually Work
Surgery isn’t always the first step. When adenoid problems are mild to moderate, several approaches can help.
Addressing underlying allergies makes a bigger difference than most people realize. Allergic inflammation swells adenoidid tissue, so controlling allergies often reduces adenoid size enough to relieve symptoms. This means identifying and avoiding allergens when possible, using saline nasal rinses to physically wash out irritants, and sometimes using allergy medications like antihistamines or nasal corticosteroid sprays.
Treating infections promptly prevents chronic enlargement. Acute adenoiditis (infected adenoids) causes temporary swelling. If you treat infections quickly and thoroughly with antibiotics when bacterial, the adenoids often return to their baseline size. Letting infections linger or recur frequently keeps adenoids perpetually swollen.
Nasal steroid sprays reduce inflammation directly. Prescription-strength nasal corticosteroid sprays (like fluticasone or mometasone) can shrink swollen adenoid tissue in some children. This works better for allergy-related swelling than for anatomically oversized adenoids, but it’s worth trying before jumping to surgery.
Watchful waiting has its place. If symptoms are mild and the child is likely to outgrow the problem soon (they’re already 6-7 years old and adenoids naturally shrink after that), doctors might recommend monitoring rather than immediate intervention. Regular checkups ensure the situation isn’t worsening.
These conservative approaches work best when symptoms are manageable and not causing significant sleep disruption, hearing problems, or developmental issues. They buy time for natural adenoidid shrinkage to occur.
When Surgery Becomes the Right Answer
An adenoidectomy—surgical removal of the adenoids—sounds intimidating, but it’s one of the most common pediatric procedures performed. Understanding when it’s genuinely necessary helps you make informed decisions.
Severe sleep apnea requires intervention. If sleep studies show significant oxygen desaturation, frequent waking episodes, or evidence of strain on the heart from breathing difficulties, that’s a clear surgical indication. Sleep apnea doesn’t improve on its own and causes real harm when left untreated.
Recurrent ear infections resistant to other treatments indicate surgery. The threshold varies, but generally 5-6 infections per year despite antibiotics, or persistent fluid lasting 3+ months with hearing loss, suggests adenoid removal could solve the underlying drainage problem.
Failed medical management after adequate trial. If you’ve tried nasal steroids, allergy control, and other conservative measures for 2-3 months without improvement, and symptoms still significantly affect your child, continuing the same approach rarely produces better results.
Adenoid-related complications have developed. Conditions like chronic sinusitis linked to blocked drainage, changes in facial/dental development from mouth breathing, or failure to thrive from eating/breathing difficulties shift the risk-benefit calculation toward surgery.
The procedure itself takes about 20-30 minutes under general anesthesia. Surgeons use specialized instruments to remove adenoid tissue through the mouth—no external incisions. Most children go home the same day and return to normal activities within a week.
What Recovery Actually Looks Like
Medical websites describe adenoidectomy recovery in clinical terms. Here’s what actually happens.
Days 1-3 are the roughest. Your child will have throat soreness, possible low-grade fever, and general crankiness. They’ll eat soft foods (ice cream, pudding, mashed potatoes) not because their throat can’t handle regular food, but because it’s uncomfortable. Keeping them hydrated matters more than convincing them to eat.
Bad breath is completely normal and temporary. The surgical site forms a whitish-gray coating (scabs) as it heals. This creates breath that smells worse than you’d think possible. It’s not an infection—it’s part of normal healing. It resolves within 7-10 days.
Some bloody saliva is expected, but heavy bleeding isn’t. Seeing pink or light red streaks in saliva is normal, especially after eating or coughing. Bright red blood flowing freely, or blood clots being spit up, requires immediate medical attention.
Energy returns gradually. Most kids feel significantly better by day 4-5. They’re back to school within a week, though contact sports and swimming wait another week to allow complete healing.
Sleep improvements can be dramatic—sometimes immediately. Many parents report their child stops snoring the very first night after surgery. Breathing becomes effortless. The difference can be shocking after months or years of struggling.
Realistic Expectations: What Surgery Fixes and Doesn’t Fix
Adenoidectomy solves specific problems extremely well, but it’s not a cure-all.
It dramatically improves nasal breathing and sleep quality. If enlarged adenoids were blocking the airway, removing them opens things up immediately. Most kids stop snoring, breathe through their noses normally, and sleep peacefully.
It significantly reduces ear infection frequency. Restoring normal Eustachian tube function through adenoid removal typically cuts ear infection rates by 50-75%. Some kids still get occasional infections—adenoidectomy doesn’t eliminate infection risk entirely—but the pattern of constant, recurring infections usually ends.
It doesn’t cure allergies. If your child’s adenoid enlargement stemmed from allergic inflammation, the allergies remain. You’ll still need to manage those separately. Surgery just removes the chronically swollen tissue that allergies kept inflamed.
It doesn’t guarantee perfect health forever. Some children need ear tubes placed at the same time because fluid has been present so long. Others might develop tonsil problems later if tonsils become the main issue. Adenoidectomy addresses adenoid-specific problems, not all throat/ear issues.
Adult Adenoidid: Yes, It Happens
Though less common, adults can have adenoid problems too.
Most people’s adenoids shrink to near-invisibility by late teens. However, some adults retain larger adenoid tissue that can cause similar symptoms to children: nasal obstruction, postnasal drip, snoring, recurrent sinus infections, and sleep apnea.
Adult adenoid problems often get missed because doctors don’t expect them. If you’re experiencing persistent nasal blockage that doesn’t respond to typical sinus treatments, chronic throat mucus, or sleep-disordered breathing, ask your ENT specialist to actually look at your adenoids with a scope. Simple examination can identify if residual adenoid tissue is contributing to your symptoms.
Adult adenoidectomy is less common than pediatric, but it’s performed when indicated. Recovery is similar, though adults sometimes experience slightly more post-operative discomfort than children.
FAQ
What is adenoidid exactly?
Adenoidid typically refers to adenoid-related problems, particularly enlarged adenoids (adenoid hypertrophy) or inflamed/infected adenoids (adenoiditis). Adenoids are lymphoid tissue pads behind the nasal cavity that trap bacteria and viruses as part of the immune system, particularly in children.
How do I know if my child’s snoring is serious?
Occasional quiet snoring isn’t concerning. Seek medical evaluation if your child snores loudly every night, has observable breathing pauses during sleep, wakes frequently, seems exhausted despite adequate sleep time, or has behavior/attention problems potentially linked to poor sleep quality.
Will my child’s adenoids grow back after surgery?
Adenoid regrowth after complete removal is rare (occurs in less than 2% of cases). If surgeons leave small amounts of adenoid tissue intentionally to preserve immune function, that remaining tissue might enlarge later, but complete surgical removal typically prevents regrowth.
Can adenoid problems cause bedwetting?
Yes, there’s a connection. Sleep apnea from enlarged adenoids disrupts normal sleep cycles and can affect bladder control. Many children with adenoid-related sleep apnea experience bedwetting that resolves after adenoidectomy, though bedwetting has multiple possible causes.
Do adenoids affect speech development?
Chronically enlarged adenoids can affect speech in two ways: chronic nasal obstruction creates a “talking through your nose” sound quality, and if they contribute to hearing problems through ear infections, that hearing loss can delay speech and language development.
Is adenoidectomy covered by insurance?
Most insurance plans cover adenoidectomy when it’s medically necessary—meaning documented sleep apnea, chronic ear infections with hearing loss, or significant nasal obstruction affecting quality of life. Coverage requirements vary, so verify your specific plan’s criteria before surgery.
What’s the difference between adenoidid and tonsillitis?
Adenoids and tonsils are different structures, though both are lymphoid tissue. Adenoids sit behind the nose at the back of the throat (not visible when looking in the mouth), while tonsils are visible on both sides at the back of the throat. Both can become enlarged or infected, sometimes simultaneously, which is why adenotonsillectomy (removing both) is common.
Moving Forward With Confidence
Adenoidid—whether you are facing the problem of enlarged adenoids disrupting sleep, the baby being sick all the time because of chronic infections, or continuous nasal congestion causing that life quality to drop—should not be a mystery or a burden anymore.
The main point is to indicate when the problems with the adenoids have changed their category from “minor annoyance” to “real health impact”. Sometimes, snoring is rarely enough to indicate sleep apnea. One or two ear infections per year do not equate to hearing being impaired by the presence of fluid all the time. Seasonal allergies causing a little bit of congestion differ from difficulties in breathing the whole year affecting one’s facial structure.
When the conservative techniques like managing allergies, nasal steroids, and prompt treatment of infections are not producing the desired results, often, the surgical options come in and make the situation turn around excellently with a relatively low rate of risk. Adenoidectomy is done routinely but that does not mean your worries are not real or that you should not deeply understand what you are going to deal with.
Always trust your observation as a parent or a patient. You are the person who can tell what “normal” conditions are for your child or yourself. The medical breathing, sleeping, or health patterns could be considered consistently wrong by the doctors and the parents might be the ones to convince them to start evaluating and only then trying surgical solutions that often deliver not only the medical symptoms but the whole quality of life improvement in case of relief.
Adenoidid may sound clinical and complicated, but its essence is nothing else than knowing when the small pads of tissue in your throat have become so big as to cause real trouble—also being aware that there are very effective solutions when they do come up.